By Amanda Pustilnik
This week, the CLBB and the Petrie-Flom Center at Harvard Law School are hosting a series of posts on how brain imaging can help the law address issues of physical and emotional pain. Our contributors are world leaders in their fields, who participated on June 30, 2015, in the CLBB/Petrie-Flom conference Visible Solutions: How Brain Imaging Can Help Law Re-envision Pain. They addressed questions including:
- Can brain imaging can be a “painometer” to prove pain in legal cases?
- Can neuroimaging help law do better at understanding what pain is?
- How do emotion and pain relate to each other?
- Does brain imaging showing emotional pain prompt us to reconsider law’s mind/body divide?
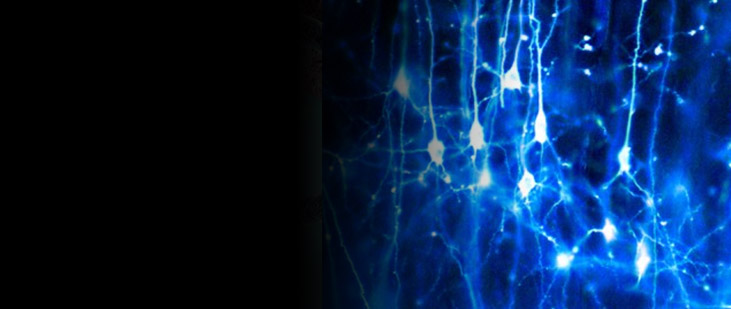
Professor Irene Tracey, D.Phil., a pioneer in pain neuroimaging and director of the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain, opened the conference with a keynote explaining what happens when the brain is in pain.
Professor Hank T. Greely, Edelman Johnson Professor of Law and Director of the Program in Neuroscience and Society at Stanford Law School, provided a keynote explaining the many implications of brain imaging for the law.
This conference was the culmination of CLBB’s year of work on pain neuroimaging and law. As the first CLBB-Petrie-Flom Center Senior Fellow on Law & Applied Neuroscience, I focused on pain because it is one of the largest social, economic, and legal problems that can be addressed through new insights into the brain. Pain imaging can be a test case for how neuroscience can contribute positively to law and culture. (Full conference video proceedings are available here.) Please read on below!
Pain is also a huge cause of suffering in the world, and it would be honorable if law and science working together could reduce that suffering, even just a little. On a human and economic level, pain is the single largest cause of disability globally and in the US. On the legal level, the US and other legal systems are not effective at evaluating physical and emotional pain, identifying its long-term effects, and sorting genuine claims from false ones.
I also am passionate about pain neuroscience on a personal level: After a routine outpatient procedure that went wrong, nearly a decade ago, my sister developed life-changing pain. The injury healed but the pain endured. This very common type of pain is inexplicable under the old model but readily explicable, and treatable, neurologically. Her years of challenge and recovery opened my eyes to the suffering of millions who endure the double burden of pain and of pain’s invisibility, which often leads to it being dismissed. This project is dedicated to her, and to everyone who has had or will have pain – which is all of us.
I hope you will tune in this week for contributions from:
This post is part of the series on pain, brain imaging, and the law sponsored by the MGH Center for Law, Brain & Behavior, the Petrie-Flom Center, and Harvard University’s Mind/Brain/Behavior Initiative. Contributors participated in the conference Visible Solutions: Now Neuroimaging Helps Law Reenvision Pain. For inquiries, please contact the organizer Amanda C. Pustilnik (@apustilnik on Twitter).