LAW LACKS A SUFFICIENT UNDERSTANDING OF PAIN
The subjective experience of pain presents challenges to the way it is understood. Dramatically varied presentations of pain from the same supposed pain-causing experience, and the presentation of indefinite (chronic) pain without clear cause, inform and exacerbate the psychosomatic narrative used to explain and adjudicate pain legally and societally. Since the time of Freud, neuroscience has elucidated a much clearer understanding of pain. Pain is an independent disease state, even if a pain “lesion” is not obvious – not an outdated symptom of something else.
Yet, this established, scientifically outdated understanding of pain remains the lens through which legal issues of pain are interpreted:
- Fetal pain, where, despite consensus that fetal perception of pain is unlikely before the third trimester, fierce legal debate around this “socially derived verifiability construct” continues to push the issue to the highest US courts.
- Torture and confinement, where US prisoners are regularly placed in conditions of isolation and confinement that may violate the Eighth Amendment and federal laws. Moreover, execution and cruel and unusual punishment in the form of torture, internationally prohibited since 1948, remain widely practiced and condoned by many nations.
- Disability law, where, when rendered unable to work by an injury or cause of pain, a claimant must prove their pain proportional to the attributed “lesion.” If an “excess” of pain is claimed, claimants may only receive disability by attributing their pain to a psychogenic disorder. About 35% of disability claims are granted; at least 10% of these claims are granted via a psychogenic disorder diagnosis.
While today’s neuroscience has not yet produced a “painometer” to measure individual pain, it can offer an understanding of pain that should succeed the psychosomatic narrative still dominant in legal and popular explanation.
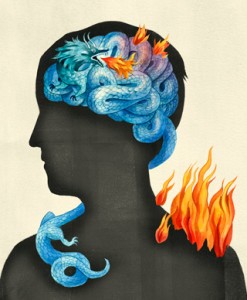
Neuroscientists understand that pain sensation begins when nociceptors – tissue sensing nerve cells – experience painful stimuli and send signals to the brain. The signals arrive in the brain and are dealt with by a network of systems and pathways whose sensitivity and efficacy vary among individuals, determining their experience of pain. This variability in individual experience of pain is similar to variability of other kinds of experiences (e.g., rollercoasters), and explains how chronic pain is developed and why different treatments are useful for different people. Using tools like fMRI, neuroscience now has the potential to map brain pathways and offer increasingly tailored treatment, explanation, and measurement of pain in the individual.
Additionally, neuroscience has a robust and useful understanding of pain that should be extrapolated to the law.
HOW CAN THE LAW REFLECT WHAT WE KNOW ABOUT PAIN?
Scientists, scholars, and policy-changers in the fields of cognitive neuroscience, psychology, neurobiology, law, and journalism have established a critical mass of resources dedicated to improving the pipeline from the science of pain to the public and the law.
International organizations such as the MayDay Fund, American Pain Society, International Association for the Study of Pain and the World Institute of Pain have been bringing together patients, clinicians and advocates to promote better research and treatment of pain long before its neurobiological origins were understood. The Pain Research Forum is the primary forum for the dissemination of new research, including neuroscience.
Pain has made its way into the public narrative through popular media. Pain is the central topic of recent news, including the Supreme Court’s decline to hear a case on fetal pain, botched executions in Texas and Oklahoma, and the Long Island Railroad disability scandal. First person accounts of pain, including former Stanford Medical School dean Phillip Pizzo’s “Lessons in Pain Relief,” Frank Porreca and Theodore Price’s “When Pain Lingers,” and syndicated medical journalist Judy Foreman’s A Nation in Pain elucidate the health crisis pain presents. The state of pain research is reviewed in the Boston Globe piece “I don’t feel your pain,” and The New York Times’ “Reading pain on a human face” highlights research on the ability to detect feigned emotion, including pain. Keith Wailoo’s Pain: A Political History, examines the history of access to treatment for pain. The video “How does your brain respond to pain?,” produced by TEDEd and eminent pain neuroscience Karen Davis, is key resource for explaining the neuroscience of pain. (These videos are also helpful). Stanford bioethicist Hank Greely’s talk “Neuroimaging, Mind Reading, and the Courts” is a primer on how neuroscience is used in the courtroom, and Colorado neuroscientist Tor Wager’s 2013 talk “Picturing pain in the brain” highlights the status of using neuroimaging to measure pain. In February 2014, leading journal Nature Neuroscience featured a special monthly issue devoted to pain, suggesting the emergence of pain as a key area of neuroscience research.
PAIN: MOVING THE AGENDA FORWARD

Pain: what are its causes, how do we measure it, and why do individual experiences of the supposed same pain-causing experience vary so dramatically? And, how do we decide how much is too much pain? The law depends on answers to these questions in order to be able to establish decent, informed legal doctrine regulating the accommodations for and limits to pain in society.
This interplay – between subjective experiences and objective measures of internal states – also has deep philosophical implications that get to the heart of how we treat fundamentally subjective constructs in both medical and forensic contexts. Will the ability to objectively measure central nervous system representations of pain impact the practice of medicine? Will the emerging understanding of pain biology change our understanding of the origins, severity and chronicity of pain? Should the science of suffering inform evaluations for disability, fitness for duty, bystander torts, or PTSD? Should neuroimaging of subjective pain be leveraged to assess “pain and suffering” in personal injury settlements?
CLBB is driving the answers to these pressing questions forward by promoting unprecedented interdisciplinary collaboration among pain scientists, legal scholars, journalists, and philosophers. The CLBB pain and suffering working group, established in May 2014, brings together experts in pain, emotion, and the law. Working group members Lisa Feldman Barrett, profiled in the Boston Globe for her work on the neuroscience of emotion, David Borsook, whose P.A.I.N. research group is leading the task of quantifying pain, and legal scholar Amanda Pustilnik, who has published numerous papers on pain in the law, and led a national conference on pain neuroimaging and the law, explore the complex intersection of the neuroscience and ethics of pain and suffering and its implications for civil and criminal law.
The group culminated its first year with a public Symposium, “Re-Envisioning Pain: How Breakthroughs on the Science of Suffering Could Revolutionize Legal Understandings & Outcomes” on February 5, 2015 at Harvard Medical School. Watch complete event video here.







