By , , , , , , , , , , , , and
Abstract:
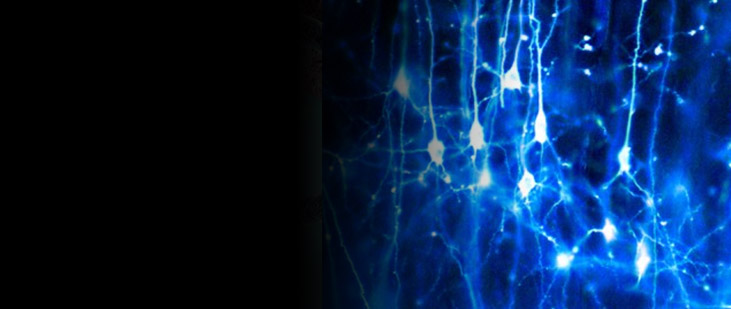
Migraine headache is uniquely exacerbated by light. Using psychophysical assessments in patients with normal eyesight we found that green light exacerbates migraine headache significantly less than white, blue, amber or red lights. To delineate mechanisms, we used electroretinography and visual evoked potential recording in patients, and multi-unit recording of dura- and light-sensitive thalamic neurons in rats to show that green activates cone-driven retinal pathways to a lesser extent than white, blue and red; that thalamic neurons are most responsive to blue and least responsive to green; and that cortical responses to green are significantly smaller than those generated by blue, amber and red lights. These findings suggest that patients’ experience with colour and migraine photophobia could originate in cone-driven retinal pathways, fine-tuned in relay thalamic neurons outside the main visual pathway, and preserved by the cortex. Additionally, the findings provide substrate for the soothing effects of green light.